Understanding Headaches & Migraines as you Transition into Menopause
Headaches are a type of neuropathic pain, which is caused by damage or dysfunction within the nervous system itself (compared to
nociceptive pain, which occurs from damage to your body tissues from an injury or accident that activates specialized nerve cells located on the surface of the skin and throughout most of the body called nociceptors). The damaged nerve cells can send signals to the brain that are interpreted and felt as pain. Neuropathic pain can be chronic – lasting more than 6 months – or it can be resolved if the underlying damage is fixed. For example, inflammation in a tissue can press on nerve cells causing them to signal pain to the brain. If the inflammation goes away – say through the use of anti-inflammatory drugs – the pressure on the nerve cells will also go away and the pain will stop.
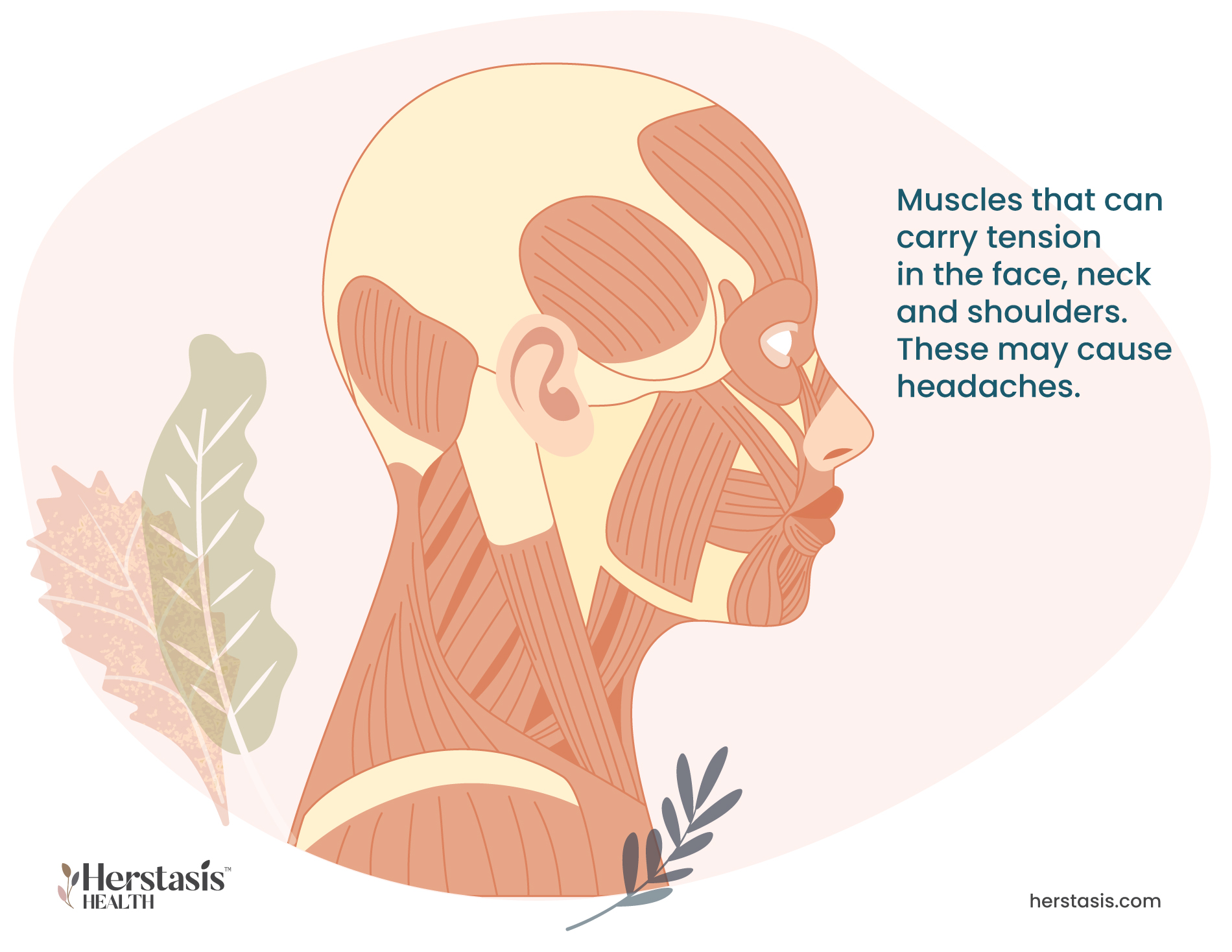
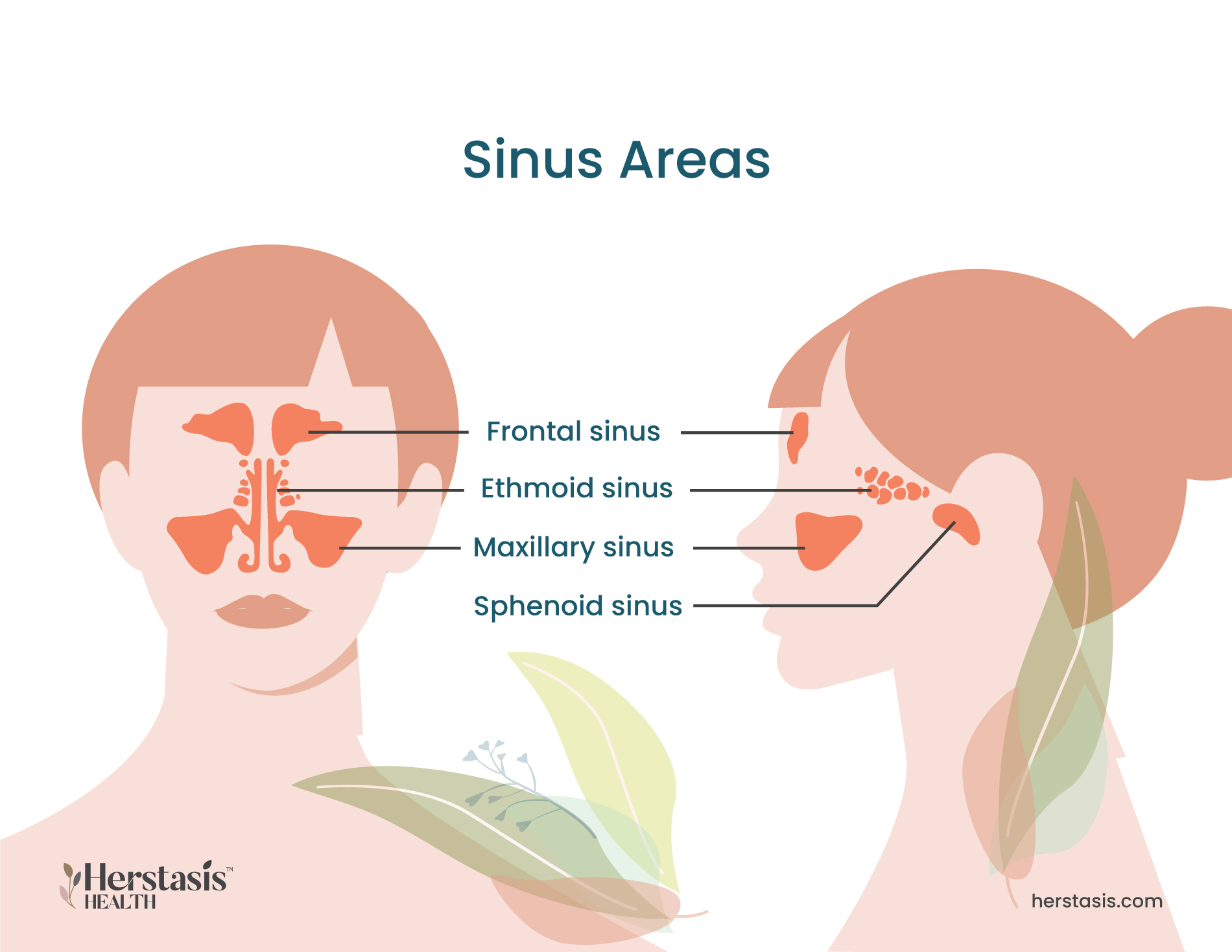
Headaches cause pain in the head, face, or upper neck, and can vary in frequency and intensity. They are classified as either primary or secondary headaches. Primary headaches are caused by the activity of or issues with pain-sensitive structures within your head. Migraine and tension headaches are examples of primary headaches. Secondary headaches are a symptom of another issue or condition, such as an infection, stress, concussion, or just drinking too much the night before. [1]
Perimenopause and headaches often occur together because the hormones estrogen and progesterone can affect headache-related neurotransmitters in the brain. This is why it is common for hot flashes and headaches to be linked. Having steady estrogen levels might improve perimenopause headaches and perimenopause migraine, as well as headache and night sweats, while having estrogen levels that dip or change can make headaches worse. [2]
There are many different types of headaches, many of which are not dangerous. However, it is important that you get emergency care if you experience any of the following:
- An abrupt, severe headache that feels like a thunderclap (possible aneurysm);
- Any headache that is accompanied by a fever, nausea or vomiting, a stiff neck, mental confusion, seizures, numbness, or speaking difficulties. These can be caused by several different issues including a stroke, meningitis, encephalitis, or a brain tumor;
- A headache after a head injury, even if it’s a minor fall or bump. This is especially true if the headache starts to worsen;
- Any sudden, severe headache that you have never experienced before; or
- A headache that gets worse over several days and changes in how you experience it. [3]
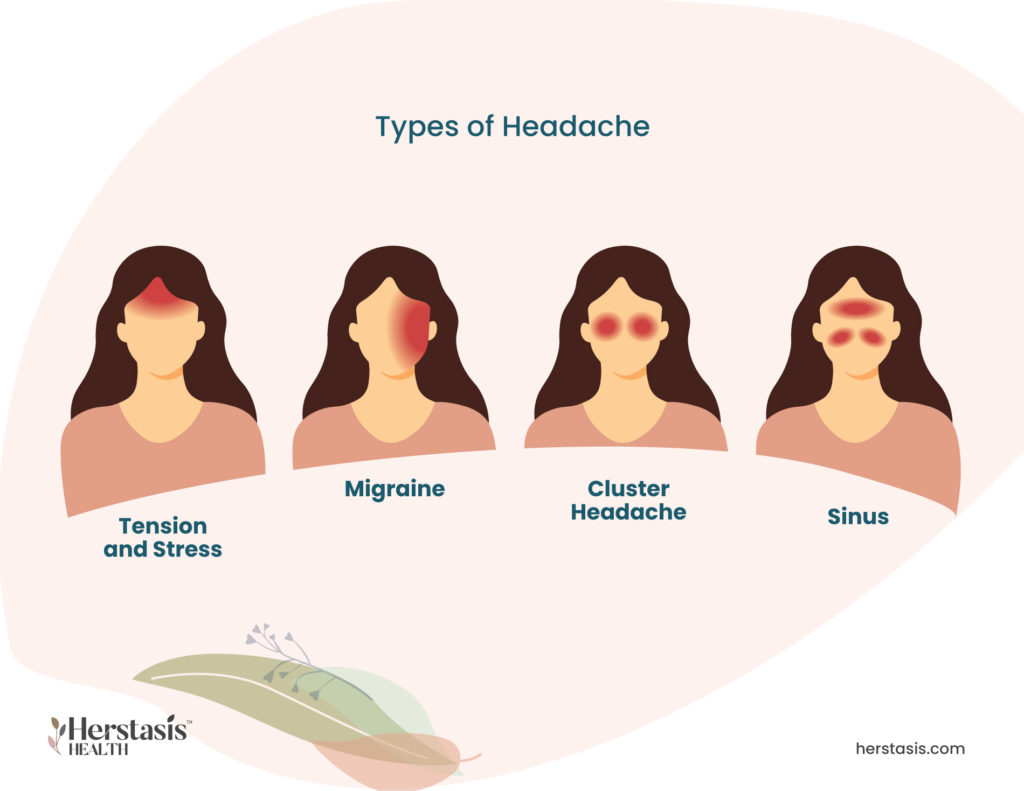
The main types of headache that can be affected by the menopausal transition are:
Self-care & Natural Remedies for Headaches & Migraines
Headaches can be awful. While headaches can have multiple causes, self care for one type of headache is very likely to help with other types of headaches. Try any of the following to see what is most effective for you and the headaches that you experience.
At home treatment for your head pain can include any or all of the following:
- Using a cold cloth or an ice pack held against the painful area on your head or neck. You can wrap the ice pack in a towel to protect your skin
- Relaxation exercises to lower stress and anxiety
- Learn and practice biofeedback techniques you to monitor and understand how your body responds to stress
- Acupuncture and or massage may help you relax
- Over-the-counter pain relievers such as ibuprofen or aspirin
- Over-the-counter allergy medications
- Practicing meditation and mindfulness exercises
- Practicing good sleep habits
- Rest in a comfortable position (whatever works to ease the pain) in a room with low sensory stimulation (low noise levels, low light levels etc.)

Therapy & Treatment for Headaches & Migraines
At age 40 find a reliable, educated primary care provider familiar with recognizing and treating symptoms of perimenopause and menopause. The North American Menopause Society provides a list of menopause practitioners here.
If you have tried self-care and your headaches are still problematic, work with your doctor to find relief with medical alternatives. The following medications may be helpful:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These are non-opioid analgesics (pain relievers) that reduce inflammation and stop the pressure of inflammation on the nerve cells, effectively stopping the pain of your headaches. Some NSAIDs are over-the-counter, such as ibuprofen, however, your doctor can also prescribe NSAIDs if necessary. [8]
- Triptans. These drugs are selective serotonin receptor agonists, which work by stimulating the production of the neurotransmitter serotonin. This acts to reduce inflammation and constricted blood vessels, both of which can stop the headache pain within hours. [9]
- Gepants. This is a new and effective type of migraine treatment that blocks a protein found throughout our bodies called calcitonin gene-related peptide (CGRP). CGRP is thought to be involved in migraines because it causes inflammation and individuals who suffer from regular migraines have excess CGRP in their blood. Gepants are unique in that they both treat existing migraines and are also known to prevent migraines from happening in the first place. At the moment, gepants are available in the U.S. but not yet in Canada. Their approval is expected during 2022. [10]
- Hormone therapy. If your headaches or migraines have changed in frequency or intensity since you entered the menopausal transition, you may want to discuss hormone therapy with estrogen as a treatment. The changing levels of estrogen during perimenopause can increase inflammation throughout the body, and inflammation can directly affect headaches and migraines.
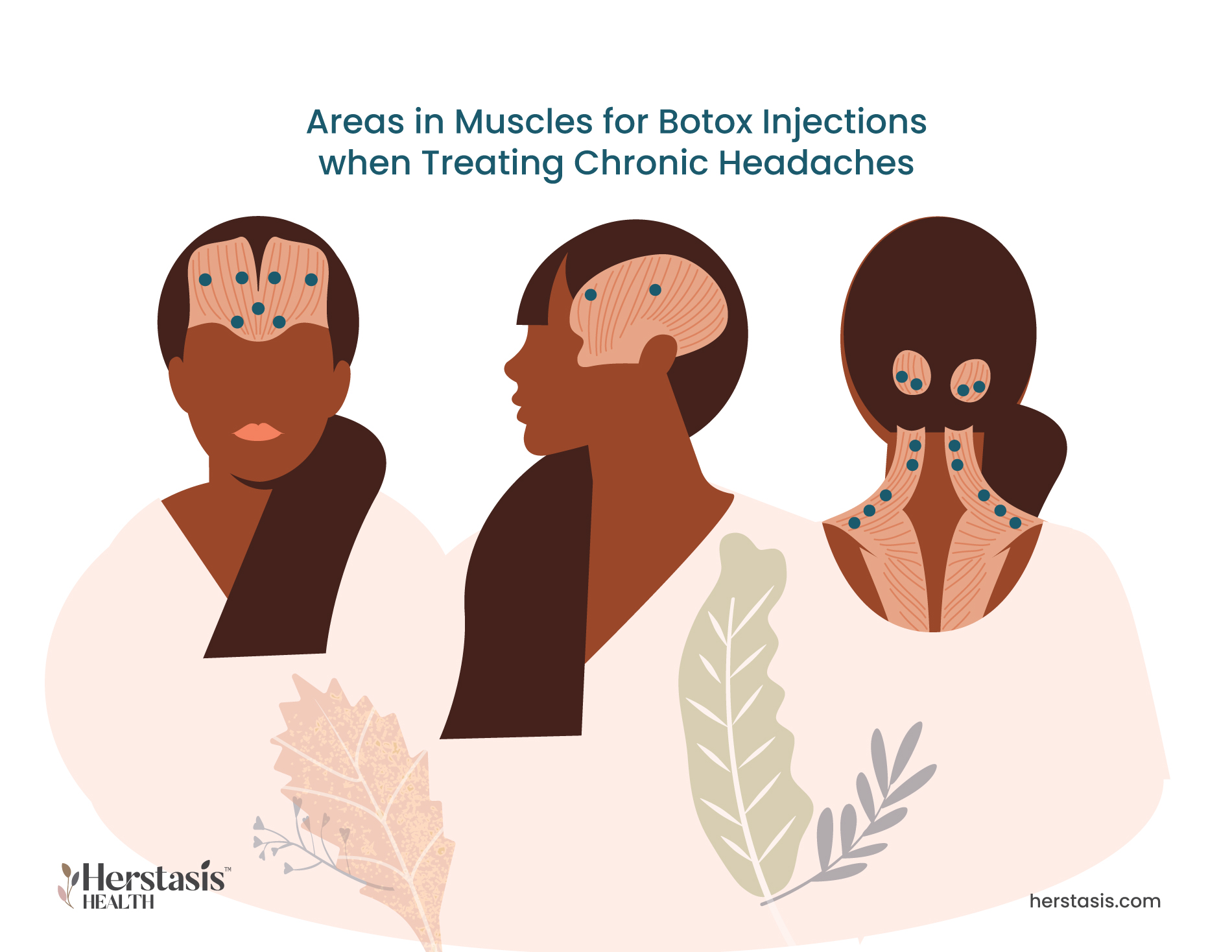
- Botox. Botulinum toxin, known as botox, can be used to treat migraines or other recurrent headaches. Botox injections block chemical signals from nerves and this usually causes muscles to relax (cosmetic botox injections relax the facial muscles and cause wrinkles to disappear). Botox used for migraine and headache relief interrupt the neurotransmitters that signal pain from the nerves to the brain. [11]
Be aware of a condition called “medication-overuse headaches”. These are headaches that result from using medications to treat headaches too frequently. This can start a vicious cycle where you get a headache, treat it with medication, the medication gives you a headache. Guidance to avoid this condition recommends treating headaches no more than 10 days per month with prescription medications and no more than 15 per month with acetaminophen or ibuprofen. [6]
While headaches are painful to experience, they are common and most individuals have had them at some point in their lives. However, it is vital that you speak to your healthcare provider and/or seek emergency care if you experience:
- An abrupt, severe headache that feels like a thunderclap (possible aneurysm);
- Any headache that is accompanied by a fever, nausea or vomiting, a stiff neck, mental confusion, seizures, numbness, or speaking difficulties. These can be caused by several different issues including a stroke, meningitis, encephalitis, or a brain tumor;
- A headache after a head injury, even if it’s a minor fall or bump. This is especially true if the headache starts to worsen;
- Any sudden, severe headache that you have never experienced before; or
- A headache that gets worse over several days and changes in how you experience it. [3]
The Science
Estrogen is linked with inflammation, and research clearly shows that lowered levels of estrogen are associated with inflammation throughout the body. [11a] Migraines are caused when the trigeminovascular system in the brain becomes inflamed. The trigeminovascular system is made up of trigeminal neurons that connect to the blood vessels in the brain and the dura. Inflammasomes are molecules that can cause the production of inflammatory cytokines, which are signaling molecules. When inflammasomes signal and stimulate the trigeminal neurons, they get inflamed and cause migraine headaches. [12] [13]
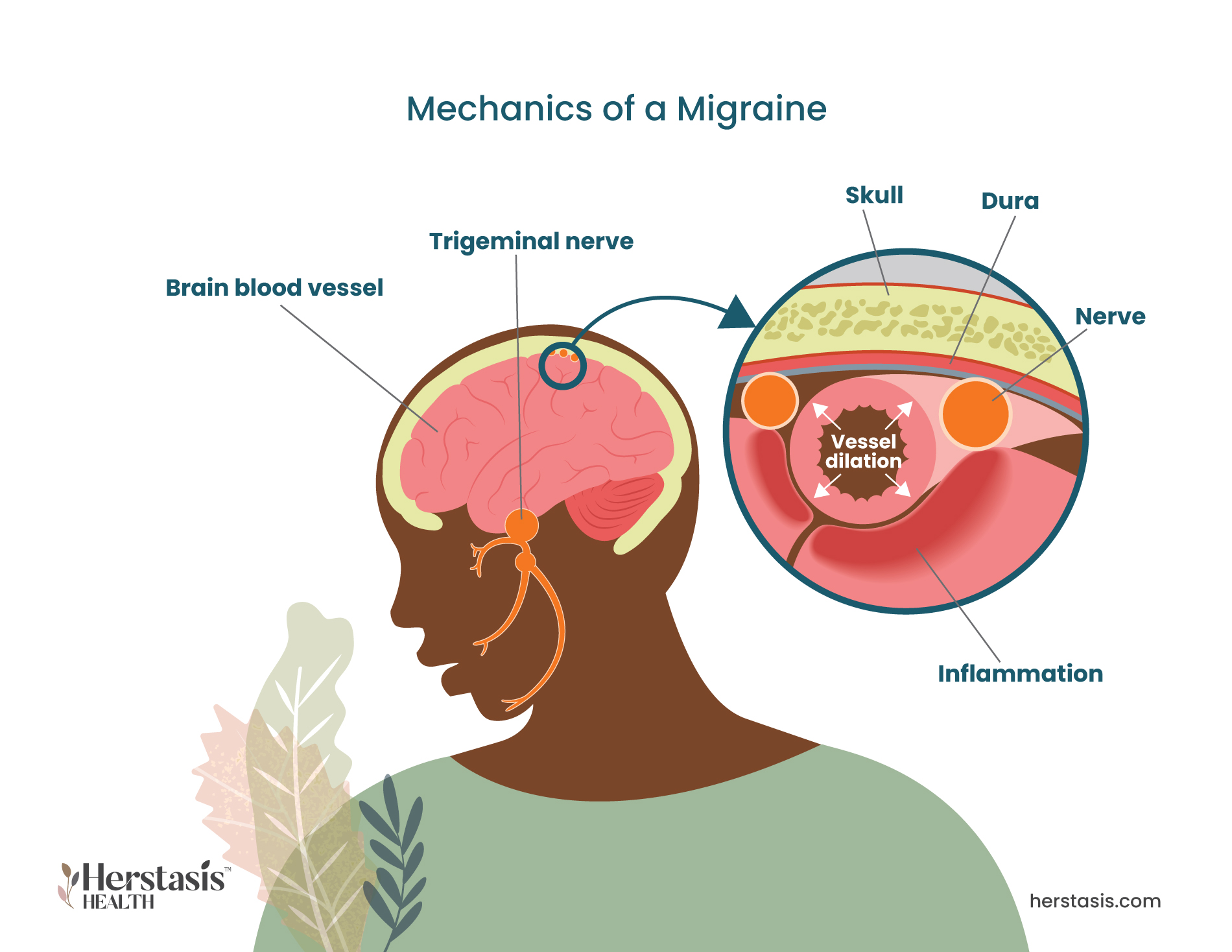
Migraines are more common in women than in men and sex hormones are believed play a large part in the difference. Fluctuations of estrogen and progesterone are believed to impact the origins and development of migraine due to the inflammatory influence of these hormones. [14] Additionally estrogen is known to influence pain sensitivity and study results are clear that women’s pain threshold and pain tolerance varies depending on the stage of their menstrual cycle. [15] Post-menopausal women with neuropathic pain, including headache pain, had significantly lower estrogen and progesterone levels as compared to control subjects. [16]
Myths & Mysteries
There are both natural treatments and medical support for headaches and migraines.
A few natural methods of relief are:
- Using a cold cloth or an ice pack held against the painful area on your head or neck. You can wrap the ice pack in a towel to protect your skin
- Relaxation exercises to lower stress and anxiety
- Learn and practice biofeedback techniques you to monitor and understand how your body responds to stress
More on Self-care & Natural Remedies for Headaches & Migraines
If you have tried self-care and your headaches are still problematic, work with your doctor to find relief with medical alternatives. The following medications may be helpful:
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Triptans.
- Gepants.
- Hormone therapy.
- Botox.
More on Therapy & Treatment for Headaches & Migraines
There are both natural treatments and medical support for headaches and migraines.
A few natural methods of relief are:
- Using a cold cloth or an ice pack held against the painful area on your head or neck. You can wrap the ice pack in a towel to protect your skin
- Relaxation exercises to lower stress and anxiety
- Learn and practice biofeedback techniques you to monitor and understand how your body responds to stress
More on Self-care & Natural Remedies for Headaches & Migraines
If you have tried self-care and your headaches are still problematic, work with your doctor to find relief with medical alternatives. The following medications may be helpful:
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Triptans.
- Gepants.
- Hormone therapy.
- Botox.
More on Therapy & Treatment for Headaches & Migraines
Headaches cause pain in the head, face, or upper neck, and can vary in frequency and intensity. They are classified as either primary or secondary headaches. Primary headaches are caused by the activity of or issues with pain-sensitive structures within your head. Migraine and tension headaches are examples of primary headaches. Secondary headaches are a symptom of another issue or condition, such as an infection, stress, concussion, or just drinking too much the night before. [1]
Learn more here
MYTH
Big stressors such as moving, starting a new job, or seeing your family over the holidays can definitely have an impact. However, the everyday stressors like traffic jams, running late to pick up the kids from daycare, or misplacing your keys are the most likely triggers for tension headaches. Not only are these stressful on their own, they can also cause you to physically tense up or clench and tighten your jaw. These in turn can trigger tension headaches or make them much more likely.
FALSE
Nope. Not true.
There are multiple treatment options available. While medications are often effective and available, they can become part of the problem if they are used too frequently.
Experiment with at-home treatments such as meditation and mindfulness practices, or dietary detox (eliminating different food groups and seeing if there is any change in your condition when you, for example, stop eating dairy or soy products). Talk to your healthcare provider about all of your options.
While this is true to a certain extent, if you suffer from frequent migraines and you take medication for them, you are at risk of a condition called medication-overuse headaches. Talk to your healthcare provider about finding alternative treatments if you suffer from frequent headaches or migraines and use medications to con
MYTH
Caffeine can trigger headaches, but it can also relieve them. Caffeine is a vasoconstrictor that causes blood vessels to narrow and restrict the flow of blood. This can help reduce headache pain. When caffeine is combined with nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen, studies have shown that the pain relief is boosted by up to 40%.
Having a cup of coffee when you feel a headache coming on may be helpful, but remember, too much caffeine, or rather the withdrawal of caffeine, can also cause headaches. If you have been drinking a lot of caffeine and you stop or slow down your consumption, your body can go into withdrawal and you can get a headache as a result. If you are planning on reducing your caffeine intake, remember to do it slowly!
FALSE
Headaches and migraines are often separated from each other based on the presence of an aura before the pain starts. The aura is usually experienced as visual disturbances or hallucinations such as flashes of light. In fact, less than one third of migraines have a distinct aura stage.
FALSE
A migraine involves more than a typical headache. In fact, headaches are often one of many symptoms of migraine. These other symptoms can include sensitivity to light and noise, nausea, weakness, and vision problems all of which can be as disabling as the headache pain.
Compiled References
[1] https://cornellpainclinic.com/conditions-treated/headaches/
[3]https://www.mayoclinic.org/diseases-conditions/cluster-headache/symptoms-causes/syc-20352080
[4] Biondi DM. Is migraine a neuropathic pain syndrome? Curr Pain Headache Rep. 2006 Jun;10(3):167-78. doi: 10.1007/s11916-006-0042-y. PMID: 18778570.
[5] https://www.healthline.com/health/menopause/pain#changes
[7] https://www.mayoclinic.org/diseases-conditions/tension-headache/symptoms-causes/syc-20353977
[8] https://www.medicalnewstoday.com/articles/179211
[9] https://www.webmd.com/migraines-headaches/triptans-migraines
[11] https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/botulinum-toxin-injectables-for-migraines
[11a] McCarthy, M., Raval, A.P. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J Neuroinflammation 17, 317 (2020). https://doi.org/10.1186/s12974-020-01998-9
[12] D. Ruthirago, P. Julayanont, J. Kim, (2017) Chapter 7.2 – Translational Correlation: Migraine, Conn’s Translational Neuroscience, Academic Press, pp 159-165,
https://doi.org/10.1016/B978-0-12-802381-5.00013-0.
[13] Kursun, O., Yemisci, M., van den Maagdenberg, A.M.J.M. et al. Migraine and neuroinflammation: the inflammasome perspective. J Headache Pain 22, 55 (2021). https://doi.org/10.1186/s10194-021-01271-1
[14] Hassany, L., Haas, J., Piccininni, M., Kurth, T., Maassen Van Den Brink, A., & Rohmann J. L. (2020) Giving Researchers a Headache – Sex and Gender Differences in Migraine Frontiers in Neurology https://doi.org/10.3389/fneur.2020.549038
[15] Wiesenfeld-Hallin Z. Sex differences in pain perception. Gend Med. 2005 Sep;2(3):137-45. doi: 10.1016/s1550-8579(05)80042-7. PMID: 16290886.
[16] Singh, A., Asif, N., Singh, P. N., & Hossain, M. M. (2016). Motor Nerve Conduction Velocity In Postmenopausal Women with Peripheral Neuropathy. Journal of clinical and diagnostic research : JCDR, 10(12), CC13–CC16. https://doi.org/10.7860/JCDR/2016/23433.9004
[16a] https://www.medicalnewstoday.com/articles/depression-headaches#causes