What is the Male Mid-life Crisis?
What is Male Menopause?
What is Andropause?
Male Mid-life Symptoms
Erectile Dysfunction
Loss of Libido
Support Your Partner
Therapy & Treatments
Self-care & Natural Remedies
Science
Myths and Mysteries
What is Male Menopause – Manopause?
Manopause. Male menopause. Midlife crisis. Andropause.
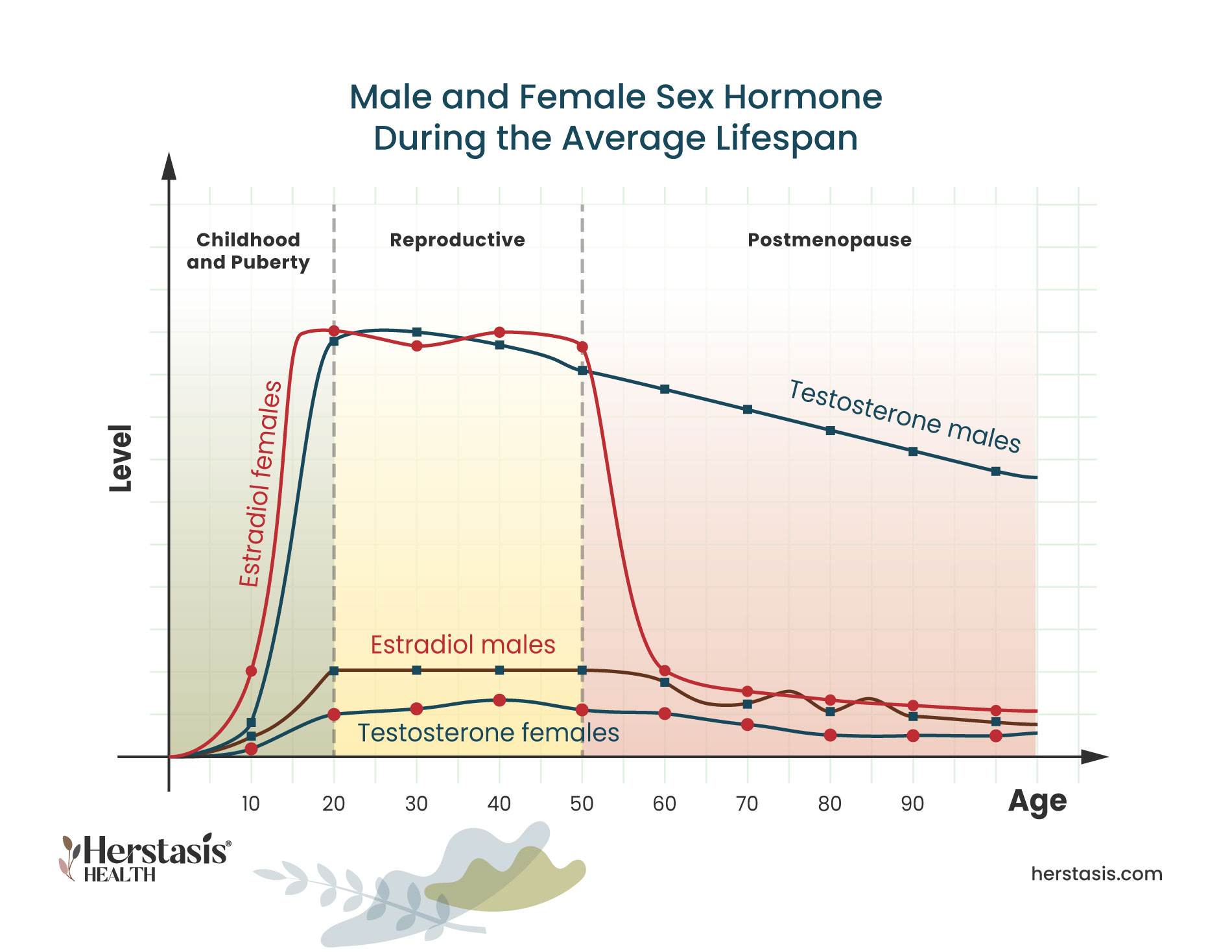
These terms are used interchangeably in the marketplace, and are confusing because men do not have the same drastic fluctuations and changes in sex hormones that underlie the female menopause.
Yet, so many men aged 40-60 experience such significant emotional and physical changes that we do need a name for this stage of life. This will allow men to start to talk openly with their family and employers about their challenges, and seek medical help when appropriate.
Whereas andropause is a true medical condition, often caused by injury, disease or medication, and there is overlap between the symptoms of andropause and midlife, we will use the terms “male midlife” and “male midlife crisis” to recognize the significance of the male experience of aging without confusing it with hormone change.
What is the Male Mid-Life Crisis?
A mid-life crisis is a relatively common experience in men, and it can be an extremely chaotic and tumultuous time. A ‘typical’ midlife crisis is defined as a period or phase of life, usually between the ages of 40 and 60, when a man begins to question their accomplishments or achievements in their lives to date. While ‘crisis’ is the common term used for this experience, in fact it is a natural process that can, in the best case scenario, include re-assessment, adjustment and acceptance. A midlife crisis can also be a factor contributing to male menopause, which is discussed here. [7] [7c]
Signs you may be experiencing a mid-life crisis as you turn 40 or older include:
General Dissatisfaction
Experiencing general dissatisfaction with life, or questioning your existing life choices
Downhill From Here
A sense that your best days are behind you, that it’s all ‘downhill’ from here
Trapped
Feeling trapped in your life
No Time
Experiencing a sense of running out of time to make any life changes or life decisions
Mood Swings
Increasing mood swings or mood changes
Increased Anger
Increasing anger at the world in general for being unfair
Targeted Anger
Increasing anger at specific individuals (such as bosses or family members) that you perceive to have held you back or been unsupportive

Withdrawing
Withdrawing from work, family, and life in general [7] [7a]
Destructive Behaviour
Exhibiting changes in behaviour, especially destructive ones that are listed below…
Destructive Behaviors
- starting or increasing drinking and illicit drug use
- starting or wanting to start an extra-marital affair
- spending money on atypical items (like a sports car or a new boat)
- spending money recklessly and/or beyond your means
- leaving or wanting to leave your family
- taking up high-risk sports and hobbies like sky-diving or rock climbing
- having more focus on and changing your appearance, by changing the way you dress, significantly increasing your workouts, or considering (or having) cosmetic surgery
- dropping long-time friends and relationships
When will my Mid-life Crisis Go Away?
It is possible to come out of your mid-life crisis better and happier than when you went into it because a mid-life crisis leads to either ‘growth or destruction’. The growth happens when men consider the underlying causes of unhappiness and dissatisfaction, and make careful and thoughtful decisions and plans to change and address those causes.
Unfortunately, you may come out of your mid-life crisis much less happy and satisfied than when you went in if you follow the destruction path. This happens when poor choices and insufficient positive actions result in radical changes such as leaving your family or spending money beyond your means.
These destructive choices may feel like they are going to improve your life and your circumstances in the moment, but instead they often destabilize your life and remove carefully built community support systems. [7b] [7c]
What Are Male Mid-life Symptoms?
Men experience real and sometimes debilitating physical and mental midlife symptoms, although they may not always report these to their healthcare provider immediately. These symptoms overlap with andropause symptoms and male menopause symptoms and often interfere with day-to-day life. They can impact not just the men experiencing them, but also their friends, family and co-workers.
The most common symptoms include:
- depression
- loss of sex drive
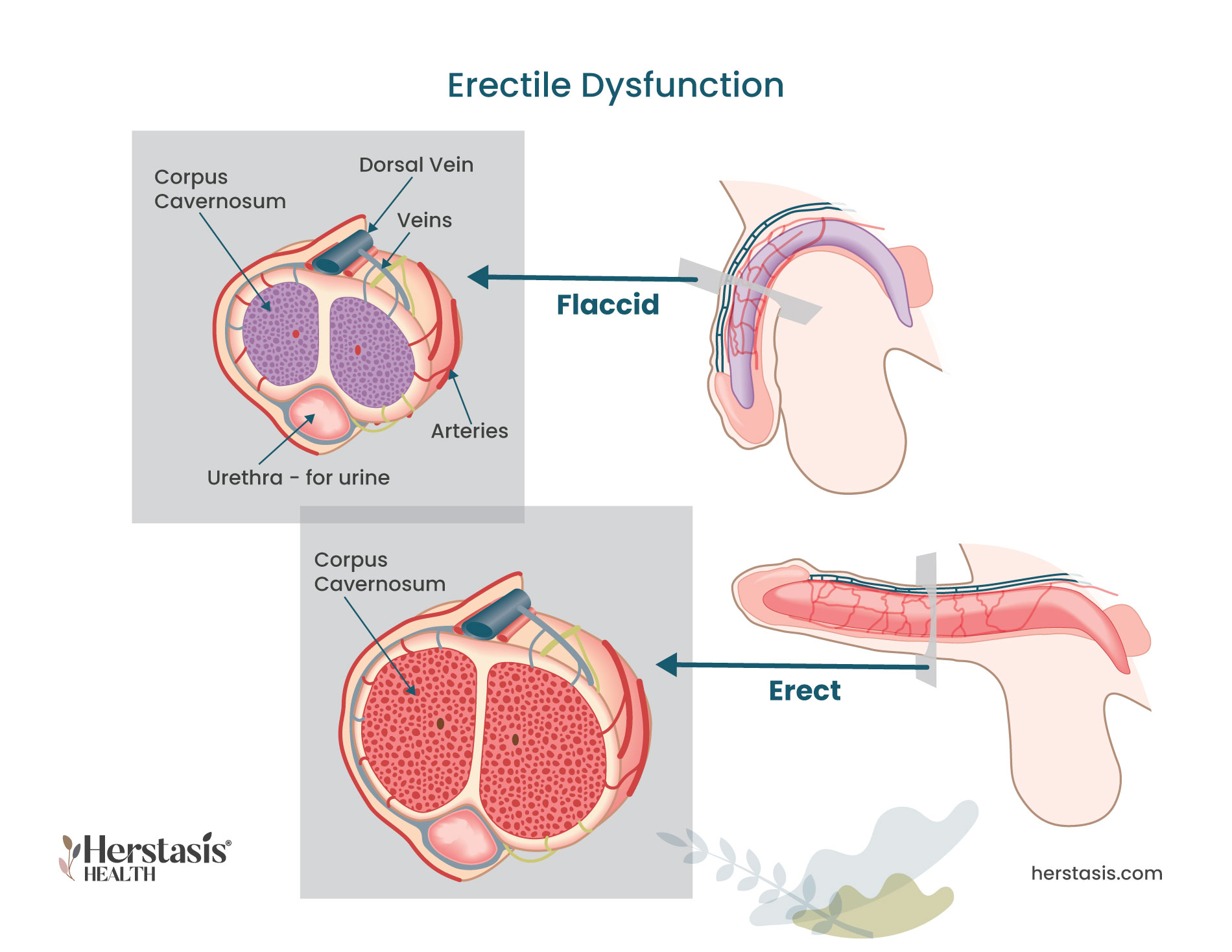
- erectile dysfunction
- mood swings and irritability
- anger
- loss of muscle mass and reduced ability to exercise
- fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
- a general lack of enthusiasm or energy
- difficulty sleeping an/or or increased tiredness
- night sweats
- hot flashes
- poor concentration and short-term memory challenges
Causes of Male Mid-Life Symptoms
It can be difficult to pin down the exact reasons for men’s mid-life symptoms. Low testosterone is often blamed, but it is rarely the primary cause unless there is a clear illness or injury to explain lowered hormone levels. Given this, it is important to recognize that lifestyle choices can be a factor, as well as psychological issues. For example, erectile dysfunction can result from stress, depression, and/or anxiety, but it is also associated with obesity, smoking, excessive drinking, and cardiovascular health problems. [1]
Common causes of male menopause symptoms include:
- stress
- anxiety
- lack of sleep
- a poor diet
- lack of exercise
- drinking too much alcohol
- smoking
- low self-esteem [1]
Night sweats in men can be caused by low testosterone, but more commonly results from anxiety and/or stress, diet, alcohol, medications, or a side effect of sleep apnea. This is true of hot flashes during the day in men as well, where the most common causes are anxiety, stress, or side effects of medication. [5][6]
Self-care and Natural Remedies for Symptoms of Male Mid-life Crisis, Male Menopause, and Andropause
It is important to understand the root causes for any symptoms you may be feeling. Know that midlife is often a time of self-reflection and self-assessment, both of which can play an important role in symptoms experienced for midlife men. Self-care for your symptoms can play an important role in helping reduce their impact, regardless of the causes.

Talk to someone you trust. Sometimes just sharing your experiences provides some perspective and can lower your anxiety or stress.
Take care of your physical body. When you eat well, get adequate exercise, and have good quality sleep, you will feel better. Full stop.
Exercise with friends. Make connections with people while you are doing something good for your body and make it a regular thing you look forward to.
Practice meditation and/or breathing exercises. Daily practices like “box breathing” help calm your mind and give you a smart tool for reducing the strength of mood swings, anger, depression or other behavioural symptoms in the moment they happen.
Journal your thoughts and feelings. Not only is keeping a journal a proven way to self-reflect and practice self-care, your journal can also help you track your symptoms. You may start to see patterns and identify situations that trigger scary and uncharacteristic feelings and behaviours. Take the time to journal things that are good as well! This can be a boost when you are feeling down or irritated.
Join a support group or a peer group. Your healthcare provider can give you a recommendation for a support group or point you to specialty care organizations that provide support for midlife men.
Practice Mind Body Wellness therapies. Refer to the Herstasis therapy page Mind Body Wellness to explore options for alternative and complementary treatments that may help you. Yoga, biofeedback and relaxation therapy, hypnosis, aromatherapy, meditative movement such as Tai Chi or Qigong, are all described in detail, as are several others. You may get inspired to try one or more of these and see if it helps any of your symptoms. [1]
Therapies and Treatments for Symptoms of Male Mid-life Crisis and Male Menopause
If you’re experiencing symptoms that could be caused by male menopause, see your healthcare provider. You will get tested for hormone levels, and you can also expect to discuss your work and personal life to see if your symptoms may be caused by problems such as stress, anxiety, poor sleep, or excess weight.

The Science
Hypogonadism and Late Onset Hypogonadism (LOH)
Hypogonadism occurs when the testes produce few or no hormones. It can be present from birth, which can cause symptoms like delayed puberty and small testes. Hypogonadism can also occasionally develop later in life, known as late-onset hypogonadism (LOH), and it is most common in men who are obese or have type 2 diabetes. When this occurs, it can cause male menopause symptoms. It is important to realize though, that LOH is not a normal part of aging, rather it is a specific medical condition. A diagnosis of late-onset hypogonadism can usually be made based on the presence of symptoms plus the results of blood tests used to measure your testosterone levels. [1]
The most common symptom of testosterone deficiency is low libido, and other common symptoms include erectile dysfunction, decreased muscle mass and strength, increased body fat, decreased bone mineral density and osteoporosis, and depression. None of these symptoms alone are specific only to low testosterone, but if any of these are present, ruling out low testosterone is the first step. It is important to exclude other common causes of these symptoms, including depression, hypothyroidism, chronic alcoholism, and use of medications such as corticosteroids, cimetidine, spironolactone, digoxin, opioid analgesics, antidepressants, and antifungal agents before making a diagnosis of LOH. [2]
Testosterone is measured in units of nanomoles (nmoles) per litre (L). A mole is an amount of a substance that contains a very large number (6 followed by 23 zeros) of molecules or atoms. A nanomole is one-billionth of a mole. A litre measures fluid volume. Testosterone can also be measured in nanograms (ng) per deciliter (dL). A nanogram is one-billionth of a gram (which is about 1/30 of an ounce) and a decilitre measures fluid volume that is 1/10 of a litre.
Testosterone can be found circulating in the body in ‘free’ form, where it is on its own, or it can be circulating in a form where it is ‘bound’ to proteins. About 98% of the body’s testosterone is bound to either SHBG (sex-hormone binding globulin), or to the protein albumin. Only 2% of the body’s testosterone is found in free form. Total testosterone, also called total serum testosterone, measures all testosterone in the blood, both free and bound forms. Free testosterone levels are significantly correlated with libido, erectile, and orgasmic function.
There is general agreement amongst various professional bodies that total testosterone levels above 12 nmol/L (350 ng/dl) does not require testosterone supplementation. There is also a consensus that patients with total testosterone levels below 8 nmol/l (230 ng/dl) will usually benefit from testosterone treatment. If the total testosterone level is between 8 and 12 nmol/l (230 and 350 ng/dl) the tests can be repeated to look only for free testosterone. This measure will help determine whether or not the individual needs additional testosterone added to their system. [2]
Myths & Mysteries
The roots of most male male menopause symptoms are usually related to lifestyle and behaviour problems. The first step for men experiencing symptoms in midlife is to check their testosterone levels in case that is a factor. But typically lifestyle changes such as improving diet, sleep, and exercise habits as well as treatment for any anxiety, stress or depression will help manage or even correct the symptoms.
The most common andropause symptoms include:
- depression
- loss of sex drive
- erectile dysfunction
- mood swings and irritability
- anger
- loss of muscle mass and reduced ability to exercise
- fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
- a general lack of enthusiasm or energy
- difficulty sleeping an/or or increased tiredness
- night sweats
- hot flashes
- poor concentration and short-term memory challenges.
The most common male menopause symptoms include:
- depression,
- loss of sex drive,
- erectile dysfunction
- mood swings and irritability
- anger
- loss of muscle mass and reduced ability to exercise
- fat redistribution, such as developing a large belly or “man boobs” (gynaecomastia)
- a general lack of enthusiasm or energy
- difficulty sleeping an/or or increased tiredness
- night sweats
- hot flashes
- poor concentration and short-term memory challenges.
Many men will experience male menopause symptoms in their midlife, starting in their late 40s and 50s.
For true diagnosed andropause, caused by low testosterone levels, the treatment is testosterone replacement therapy (TRT). Many men experiencing andropause symptoms, however, are not actually low in testosterone. In these cases, lifestyle changes such as improving diet, sleep, and exercise habits as well as treatment for any anxiety, stress or depression will help manage or even correct the symptoms.
Yes, they can be. They may be caused by low testosterone, but more commonly they result from anxiety and/or stress, medication side-effects, alcohol consumption, diet, or a side effect of sleep apnea.
Yes, they can be. They may be caused by low testosterone, but more commonly they result from anxiety and/or stress, medication side-effects, alcohol consumption, diets, or a side effect of sleep apnea.
Compiled References
[1] https://www.nhs.uk/conditions/male-menopause/
[2] Singh P. Andropause: Current concepts. Indian J Endocrinol Metab. 2013 Dec;17(Suppl 3):S621-9. doi: 10.4103/2230-8210.123552. PMID: 24910824; PMCID: PMC4046605.
[3] https://www.merithealthcentral.com/health-library/128
[4] https://www.webmd.com/men/guide/male-menopause
[5] https://www.healthline.com/health/what-causes-night-sweats-in-men#common-causes
[6] https://www.healthline.com/health/mens-health/hot-flashes-men#symptoms
[7] https://www.forbes.com/health/mind/midlife-crisis/
[7a] https://www.webmd.com/men/features/mens-midlife-crisis
[7b] https://psychcentral.com/lib/midlife-crises-affecting-men-and-families
[7c] Infurna FJ, Gerstorf D, Lachman ME. Midlife in the 2020s: Opportunities and challenges. Am Psychol. 2020 May-Jun;75(4):470-485. doi: 10.1037/amp0000591. PMID: 32378943; PMCID: PMC7347230.
[8] https://www.healthline.com/health/cbt-techniques
[9] https://www.nimh.nih.gov/health/topics/anxiety-disorders#part_2225
[10] https://www.psychologytoday.com/ca/basics/anger
[11] https://www.medicalnewstoday.com/articles/cognitive-restructuring
[12] https://mantracare.org/therapy/anger/anger-management-counseling
[13] https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction
[14] https://my.clevelandclinic.org/health/drugs/10053-vacuum-constriction-devices
[15] https://www.urologyhealth.org/urology-a-z/e/erectile-dysfunction-(ed)
[17] https://www.mayoclinic.org/healthy-lifestyle/sexual-health/expert-answers/loss-of-sex-drive
[18] Nandy PR, Singh DV, Madhusoodanan P, Sandhu AS. Male Andropause : A Myth or Reality. Med J Armed Forces India. 2008 Jul;64(3):244-9. doi: 10.1016/S0377-1237(08)80105-0. Epub 2011 Jul 21. PMID: 27408157; PMCID: PMC4921612.
[19] Bhasin S, Valderrábano RJ, Gagliano-Jucá T. Age-Related Changes in the Male Reproductive System. [Updated 2022 Feb 10]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278998/
[20] https://www.mayoclinic.org/healthy-lifestyle/mens-health/in-depth/male-menopause/art-20048056
Not AI generated.
Original content, last updated March 14, 2023.
© 2024 Herstasis® Health Foundation