Understanding Vaginal Changes
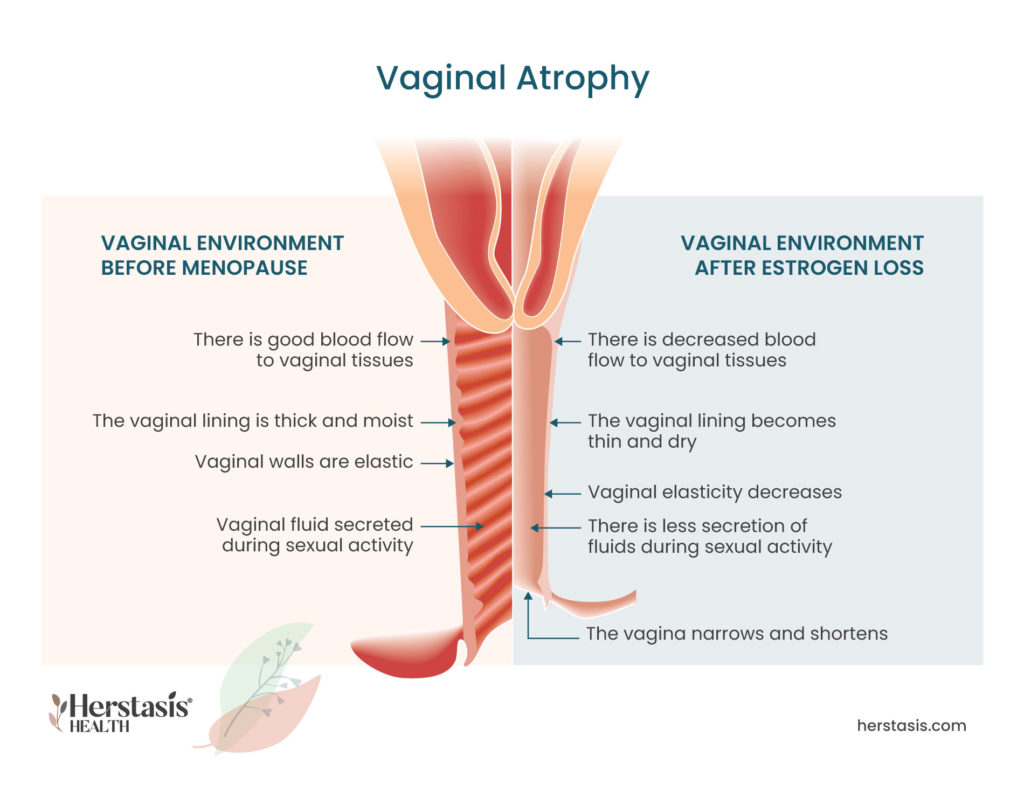
During the menopausal transition, the state of the vagina often changes. The tissues in the vagina weaken, get thinner, dryer, and may get inflamed, causing pain, burning, or discharge. Vaginal dryness and pain are symptoms of vaginal atrophy (atrophic vaginitis) that occur as a result of lowered estrogen levels. [1]
Download
Normal vaginal function includes all of the following:
Discharge:
-
- All females will experience vaginal discharge, which is the name for any substance that exits the body through the vagina. The cells in the muscular tissue lining the vagina secrete mucus, which makes the walls slippery. This mucus also protects against bacteria and yeast overgrowth.
Normal daily vaginal discharge includes a small amount of vaginal lubricants, cervical mucus, and sexual arousal fluid. If you are experiencing excessive amounts of discharge, or discharge with a strong odour or a different colour than normal, see your healthcare provider as these can be signs of other issues, including infections, that need to be immediately treated. [2]
Odor:
-
- Normal vaginal odor is mild and may occasionally be so mild that there is no apparent smell at all. While this does vary from individual to individual, strong odors from the vagina are not typical. If you do notice a change in the odor ‘down there’, especially if you have other vaginal symptoms such as itching, burning or changes to your normal discharge, talk to your healthcare provider, as you may have an infection or other condition that needs treatment.
-
- Vaginal odors are known to vary throughout the menstrual cycle, meaning there is a hormonal component to them. If you notice a change in your vaginal odor, it could be caused by a number of other factors including your changing hormones or even your diet. [3]
Dryness:
-
- Estrogen ensures that the cells in the vagina are elastic and that the walls of the vagina are thick and healthy. When estrogen levels drop, the walls of your vagina can become dryer than your normal amount of lubrication. This is one of the signs of a common female aging symptom called vaginal atrophy, where the lowered estrogen also causes the walls of the vagina to become thin and inflamed.
-
- Perimenopause, another name for the menopausal transition, is not the only possible cause for lowered estrogen levels. If you have recently experienced childbirth, are breastfeeding, undergoing cancer treatment, or experiencing any condition that requires estrogen-blocking drugs, you may also experience vaginal dryness. In these cases, when estrogen levels return to normal, the vaginal atrophy will correct itself. In the case of perimenopause, estrogen levels will continue to drop until they stabilize at a lower level permanently in menopause, meaning that most women will experience vaginal atrophy as they age.
-
- Non-hormonal factors can also cause vaginal dryness. The most common causes are some cold and allergy medications, some antidepressants, or a condition called Sjögren syndrome. This is an autoimmune condition resulting in a dry mouth and eyes, and on some occasions, vaginal dryness. [1] [4] [5] [6] [7]
Pain:
-
- Changes in the vagina during perimenopause can also result in pain, including pain during sex, after orgasm, and/or during urination, as well as other uncomfortable sensations such as burning and itching. Refer to Sexual Changes for more detailed information on pain during sex, and Urinary System Changes for more detailed information on pain during urination. [8] [9]
Women may be very reluctant to speak up and act on vaginal issues due to embarrassment and negative feelings about aging. However, these are conditions that can often be treated easily at home and with the help of a medical practitioner.
Self-care for Vaginal Changes
To address changes to your vagina, including vaginal atrophy resulting in vaginal dryness, at home you can:
- Use over-the-counter water-based lubricants to hydrate the walls of your vagina. This can also help reduce vaginal infections.
- Stimulate the muscles of and increase the blood flow to the vaginal wall with vaginal sex and masturbation, as this helps keep your vaginal tissues healthy.
- Avoid vaginal intercourse when experiencing pain and dryness, as this can result in tearing delicate tissues and may lead to infections.
- Never try to ‘clean’ or deodorize your vagina by inserting or using any herbal products, douches, deodorants, chemicals, soaps, cleansers, perfumed products, or steam. Your vagina has a natural balance of conditions, including pH (acidity) and natural bacteria, and using external products will disturb this balance. When this happens, it is likely that any odors or discharge you have will get worse and you may experience other unpleasant symptoms such as irritation and burning. Your natural and normal vaginal secretions and environmental conditions (including temperature) are the only safe ‘cleansers’ you need.
- Seek medical care if you notice increasingly strong odor, increased vaginal pain, or changes in discharge. [5] [6] [10]

Therapy for Vaginal Dryness and Urine Leakage
At age 40 find a reliable, educated primary care provider familiar with recognizing and treating the symptoms of perimenopause and menopause. The North American Menopause Society provides a list of menopause practitioners here.
The effects of menopause-related vaginal thinning and dryness can often be mitigated with over-the-counter (meaning: not needing a prescription to purchase), preferably water-based lubrication products, gentle Kegel exercises, and safe and effective HT with estrogen. [11]
You can try over-the-counter vaginal moisturizers and lubricants to help increase the moisture in the vagina. If you are using a lubricant, which is typically applied just before intercourse and reduces vaginal pain, check to see if the product contains any petroleum (like petroleum jelly). If you are in the menopausal transition there is still a chance of pregnancy, and petroleum based products can break down latex used in condoms.
If your vaginal dryness is caused by low estrogen levels, your healthcare provider may prescribe topically (locally) applied hormone therapy (HT). Locally applied HT can also help to reduce the incidence of urinary tract infection (UTI).
There are three methods of applying vaginal estrogen:

The Science
Hormones are substances that are produced in your body and then move to certain tissues to stimulate them to do an action. The hormone estrogen is responsible for stimulating cells in the vaginal wall to produce the lubricating mucus. During the menopausal transition, estrogen levels start to drop and this can lead directly to less lubrication in the vagina.
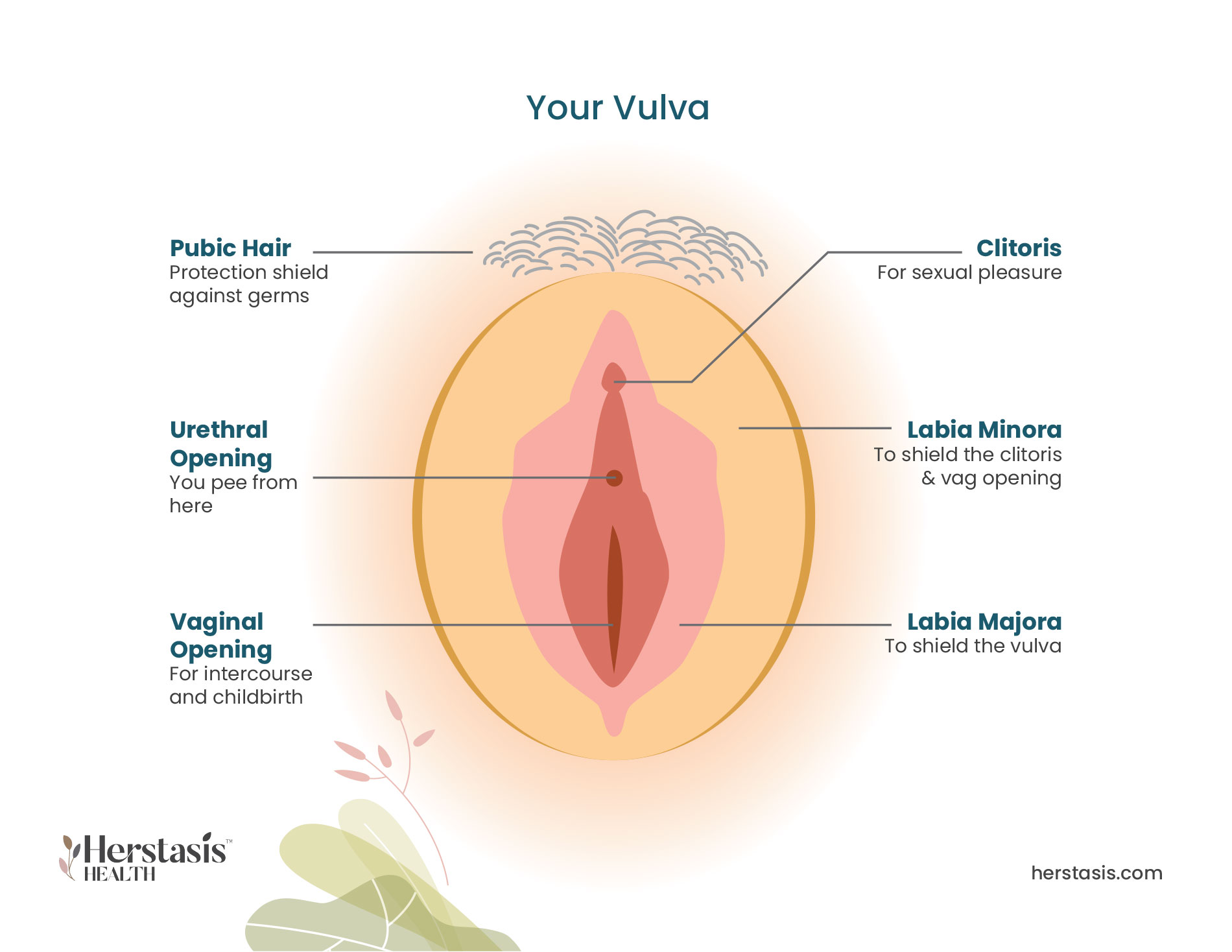
If you are experiencing vaginal dryness, you may also experience a dry and irritated vulva due to having less moisture overall up inside the vagina. As well, you may also have to urinate more frequently and could have repeated urinary tract infections (UTIs). This group of symptoms is common during menopause, and it is called the genitourinary syndrome of menopause (GSM). More information on GSM is provided below. [1] [7]
Genitourinary Syndrome of Menopause (GSM)
Changes to the vagina usually occur at the same time as changes in the urinary tract, so they have recently been combined into a single category – genitourinary syndrome of menopause (GSM). GSM covers a variety of changes to the genitourinary tract – particularly the urethra, vagina and vulva. Vaginal atrophy and urinary incontinence (UI) are the most common symptoms of GSM, affecting 40-50% of midlife and aging women. [6] [9]
Signs and Symptoms of GSM
| Vagina | |
| – | vaginal dryness |
| – | irritation / burning / itching |
| – | changes to vaginal discharge |
| – | thinning / graying pubic hair |
| – | vaginal / pelvic pain and pressure |
| – | vaginal prolapse (top of the vagina falling into the vaginal canal) |
| Urinary System | |
| – | painful urination |
| – | urgency incontinence |
| – | stress incontinence |
| – | frequent / recurring urinary tract infections |
| – | urethral prolapse |
| Sexual | |
| – | painful sex |
| – | bleeding after sex |
| – | decreased orgasm |
| – | loss or reduction in libido |
| – | pain after orgasm (dysorgasmia) |
Statistics
Yes, the vaginal atrophy part of GSM can be helped by regular sexual activity with or without a partner! Increasing blood flow to the vagina will help keep the tissues healthy. Bladder training and strengthening the pelvic floor muscles with Kegels are helpful to naturally manage urinary incontinence. While these may not be enough to completely manage GSM, they are a good start.
Unfortunately, no. The Genitourinary Syndrome of Menopause is a chronic progressive condition related to aging and reduced levels of estrogen. Menopause Hormone Therapy (MHT) can be highly effective to slow the progression of GSM. Check with your healthcare provider.
MYTH
The inside of your vagina is a carefully balanced natural environment with a unique microbiome (good bacteria and other microorganisms, just like in your gut) that works to keep it healthy. It is also a very sensitive area that can be easily harmed. Steam is very hot (by definition!) and it can easily burn the vulva and the interior of the vagina (ouch!). The herbs that are used in the steam or rinse can also cause problems if they create an imbalance in the microbiome that causes bacterial or yeast infections. There is also a possibility that bacteria can get introduced into the vagina from the equipment being used. Not recommended.
If your vaginal dryness is caused by low estrogen levels, your healthcare provider may prescribe topical estrogen therapy. There are three methods of applying vaginal estrogen:
- Ring: You or your doctor can insert a soft, flexible ring into your vagina. It releases estrogen directly to the vaginal tissues. The ring lasts about three months so it will need to be replaced regularly.
- Tablets: These tablets are inserted into your vagina with a disposable applicator.
- Cream: The cream is inserted into your vagina using an applicator.
There are over-the-counter vaginal moisturizers as well. Speak to your pharmacist or your healthcare provider to get a recommendation. Water-soluble lubricants (such as Astroglide or K-Y Jelly) can also be used on an as-needed basis. Non-water-soluble lubricants, such as Vaseline, are not recommended if you are using condoms for either contraception or for prevention of STIs because they can weaken latex and reduce the effectiveness of the condom. [5]
During the menopausal transition, the state of the vagina often changes. Vaginal dryness and pain are symptoms of vaginal atrophy (atrophic vaginitis) that occur as a result of lowered estrogen levels. The tissues in the vagina weaken, get thinner, dryer, and may get inflamed, causing pain, burning, or discharge.
The lining of the outer urethra is estrogen-dependent. During the menopausal transition, this lining thins and may become weaker than the pressure in the bladder. It is this imbalance that leads to involuntary loss of urine.
Check out the science here
FALSE
Oh, please.
A national study of 5,045 older women [11] showed the following:
| Sexual activity among older US women | |||||
| Age (years) | 50-59 | 60-69 | 70-79 | 80+ | |
| Masturbated in previous year | 54% | 46% | 36% | 20% | |
| Had intercourse (penis-vagina) in previous year | 51% | 42% | 27% | 8% | |
| Received oral sex in previous year | 34% | 25% | 9% | 4% | |
FALSE
No, there are many safe and effective non- prescription medications that can be used to lubricate your vagina. A vagina is a muscle, and it needs exercise.
FALSE
Vaginal healthy aging can be had by using non-prescription lubes, HT with estrogen, and regular exercise with masturbation and intercourse.
Compiled References
[1] The North American Menopause Society. (n.d.). Changes in the Vagina and Vulva. Retrieved July 11, 2021, from https://www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva
[2] https://health.clevelandclinic.org/vaginal-discharge-mean/
[3] https://www.mayoclinic.org/symptoms/vaginal-odor
[4] https://my.clevelandclinic.org/health/symptoms/21027-vaginal-dryness
[6] Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020 Apr 8;12(4):e7586. doi: 10.7759/cureus.7586. PMID: 32399320; PMCID: PMC7212735.
[7] Krause, M., Wheeler, T. L., 2nd, Richter, H. E., & Snyder, T. E. (2010). Systemic effects of vaginally administered estrogen therapy: a review. Female Pelvic Medicine & Reconstructive Surgery, 16(3), 188–195. https://doi.org/10.1097/SPV.0b013e3181d7e86e
[8] https://www.medicalnewstoday.com/articles/326977
[9] https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy
[10] https://health.clevelandclinic.org/vaginal-steaming/
[11] Dumoulin, C., Cacciari, L. P., & Hay-Smith, E. (2018). Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. The Cochrane database of systematic reviews, 10(10), CD005654. https://doi.org/10.1002/14651858.CD005654.pub4