What are Menopausal Allergies?
Allergies is a broad term that describes what happens when your immune system reacts to a foreign substance as if it is harmful, even though it isn’t. Pollen, shellfish, insect bites, penicillin, red wine – the list of possible allergens, or substances that cause an allergic reaction, is long. Allergens can be inhaled (through the nose), ingested (through the mouth), or absorbed (through your skin or eyes). Allergies can affect anyone of any age, race or socioeconomic status. Allergic reactions are one of the most common chronic health conditions across the globe. [1]

Allergies can start at any age, and can also stop at any age. Typically, however, seasonal allergy sufferers (those allergic to grass or plant pollens that occur for one season each year) develop symptoms between the ages of two and 20. It is very possible, however, for allergies to any of hundreds of potential allergens to start later in life. There is no clear understanding of why this happens, but adult triggers can include:
- being exposed to allergens when your immune system is overloaded, for example, if you are already sick, are pregnant, or experiencing perimenopause (when hormonal fluctuations can increase inflammation throughout our body);
- not having had significant exposure to an allergen when you were younger, so when you do have enough exposure the allergic reaction occurs;
- being exposed to new allergens, for example if you try a new perfume, if you move to a new part of the country with different plant pollens from the ones your body is used to, or if you get a new pet, of a type you haven’t had before.
Allergies and asthma often occur together in a condition called allergic asthma or allergy-induced asthma. In this case, the same substances that activate your allergy symptoms, such as pollen, pet dander, or specific food reactions, also cause asthma. [2]
While most allergic reactions to substances are simply annoying, they can also be life-threatening. Anaphylaxis, or an anaphylaxis reaction, happens when your immune system releases a flood of chemicals to combat the ‘invading’ allergen. These can cause you to go into shock where your blood pressure suddenly drops and your airways narrow, making it difficult or impossible to breath. [3]
Self-care & Natural Remedies for Allergies
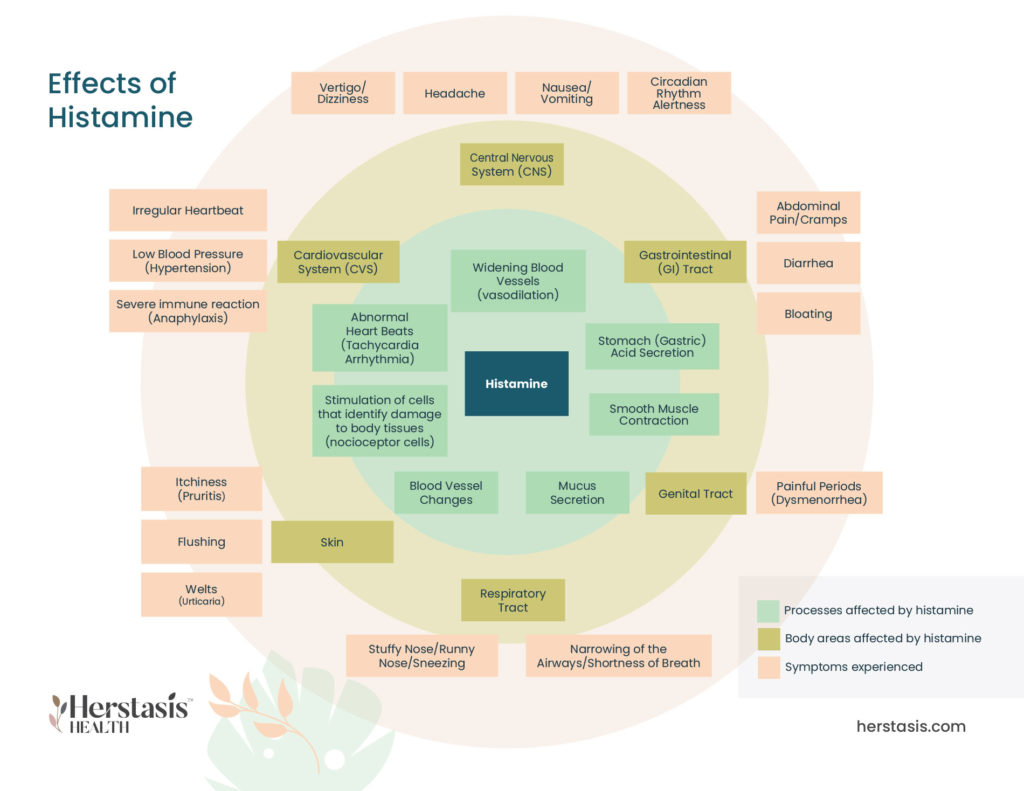
The common symptoms of allergic reactions are caused by a chemical, called histamine, that is released by your immune system when it is trying to protect you. Managing your allergies is a combination of reducing your exposure to allergens and also reducing the amount of histamine that is circulating in your system. The Science section below provides detailed information about histamine and how it affects your systems.
Histamine is created when your body identifies allergens, which are substances that your immune system thinks are dangerous to your health. The first step in controlling allergies is to avoid the allergen, if possible. This is easy if you know what the allergen is and you know where it is so that you can avoid it. In many cases, however, this is not possible because you can’t always control your environment.
If you have tried to avoid allergens and are still suffering, a good first step is to try to reduce the amount of histamine circulating in your system. Many of the treatments for allergies focus on reducing histamine levels. Histamines are not just produced in your body – they are also found in or stimulated by many common foods and drinks. Reducing histamine levels can be done by lowering your intake of histamine-containing foods and avoiding histamine- stimulating foods (foods that increase the production of histamine in your body). [4] [5]

- alcohol
- bananas
- tomatoes
- wheat germ
- beans
- papaya
- chocolate
- citrus fruits
- nuts, specifically walnuts, cashews and peanuts
- food dyes and other additives [6]
- red wine and champagne
- hard (aged) cheese
- avocado
- smoked or canned fish
- shellfish
- soy sauce
- deli meats
- yeast
- bananas
- spinach
- dried fruit
- dried nuts
- bone broth and fish stock
- vinegar and fermented foods such as sauerkraut
- chocolate [6]
- fresh meat and freshly caught fish
- non-citrus fruits
- eggs
- gluten-free grains, such as quinoa and rice
- dairy substitutes, such as coconut milk and almond milk
- fresh vegetables except tomatoes, avocados, spinach, and eggplant
- cooking oils, such as olive oil [6]
If your favorite foods are on these lists, it can be depressing to imagine a lifetime limiting your intake. However, you can try a detoxifying approach, where you remove all of the possible trigger- and source-foods until your symptoms stabilize, and then begin to add your favorites back in one at a time. This will allow you to identify those foods that have an impact on YOUR system, as it is unlikely that all of the foods on this list will have the same effect on you.
Therapy & Treatment for Allergies
At age 40 find a reliable, educated primary care provider familiar with recognizing and treating symptoms of perimenopause and menopause. The North American Menopause Society provides a list of menopause practitioners here.
Allergies are a complex reaction to many possible allergens. It is imperative that you talk to your healthcare provider about your allergies and make sure they are aware of any steps you are taking (such as reducing certain foods, using antihistamines, etc.) There are some medical treatments for allergies, but they vary widely depending on the allergen and need to be tailored to fit your circumstances. Your healthcare provider can prescribe or recommend (if they are over-the-counter) some allergy medications.
If your allergies are severe, or have become severe, immunotherapy may be helpful. This treatment involves having a series of injections that contain purified allergen extracts. These injections are taken over a period of years and are usually used to treat hayfever, allergic asthma, conjunctivitis as a result of allergens or stinging insect allergies. Allergy shots are not used to treat food allergies. The best option for people with food allergies is to strictly avoid that food.

Considerations about allergy shots include:
- Length of allergy season and severity of your symptoms
- How well medications and/or environmental controls are helping your allergy symptoms
- Your desire to avoid long-term medication use
- Time available for treatment (allergy shots requires a significant commitment)
- Cost, which may vary depending on region and insurance coverage [7][8]
Your healthcare provider may also suggest increasing the levels of the enzyme diamine oxidase (DAO) that breaks down histamine in your system. This is a response to histamine intolerance (where you have high levels of histamine circulating in your body all the time), rather than ordinary allergies, however, the result can be the same – higher levels of DAO means lower levels of histamines. Increasing DAO enzyme levels can be achieved with dietary supplements. Taking any supplements should only be done with the approval of your healthcare provider as many supplements contain ingredients that can have a profound effect on other body systems or interfere with medications that you are already taking.
If you have had, or are concerned about having an extreme allergic reaction, called anaphylaxis, you should consult your healthcare provider and consider carrying emergency epinephrine. An epinephrine shot, in the form of a EpiPen or other pre-filled injectors, should be available for use – it will reduce your immediate reaction long enough for you to get emergency treatment.
The Science
Immunity
Your body is constantly working to protect you from external pathogens like bacteria and viruses. To do this, your body mounts an immune response that can come via several different pathways. Your immune response can be either innate (that you were born with), or adaptive or acquired (immunity following exposure to the pathogen). Your innate immune system includes physical barriers (like your skin), chemical barriers (like tears), and cellular barriers (like general cellular immune responses that identify and destroy any substance that is a potential pathogen). Adaptive, or acquired immunity develops during your lifetime in response to a specific pathogen. [9]
Download PDF
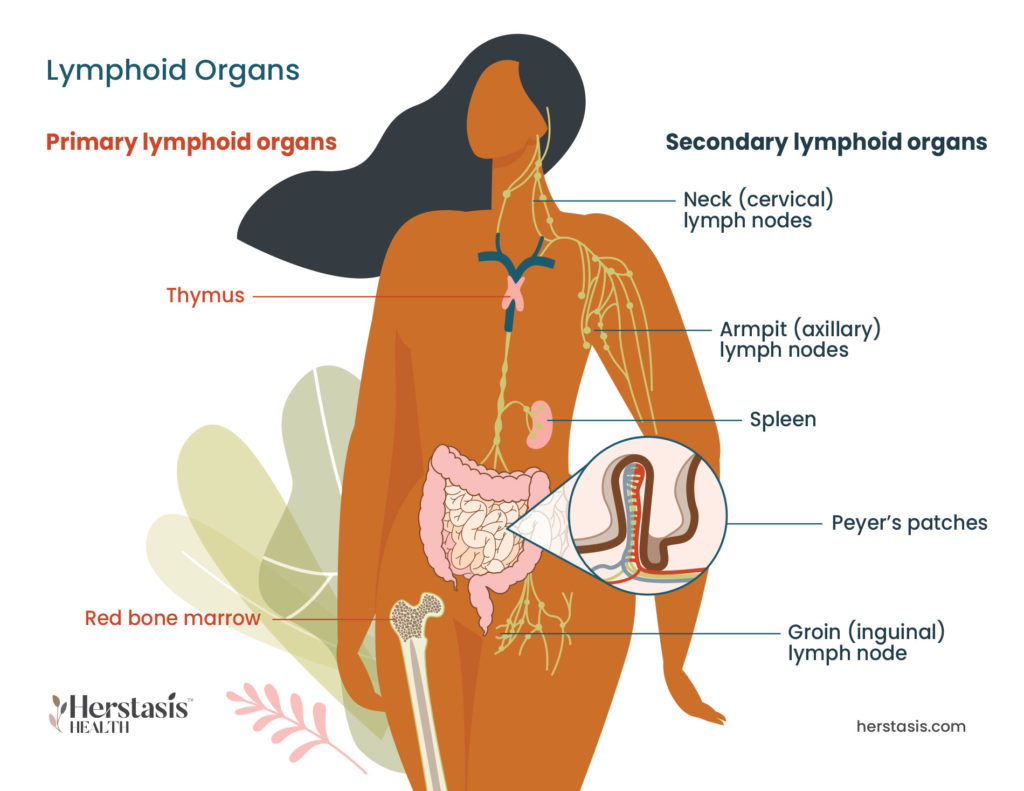
The adaptive immune response involves special lymphocytes called T and B lymphocytes, both of which mature in the bone marrow and produce antibodies (a specialized protein cell) in response to the antigens (a substance that causes the body to make a specific immune response to allergens, for example).
When a B lymphocyte (or B cell) meets up with an antigen it doesn’t recognize, it makes antibodies that are specific to the antigen, like a customized defender that will only respond to a specific invader. Not only do B cells produce the antibodies, they also create memory cells. These survive for long periods of time (decades or in some cases, your whole life) with the sole purpose of detecting specific pathogens in the future.
T lymphocytes, or T cells, originate in the bone marrow and mature in the thymus. T cells work to remove the pathogens from the body. When a pathogen enters a cell in the body, the T-cells notify the B-cells to make an antibody, and also activate a specialized type of T cell called a killer T cell that kills any cells invaded by the pathogen. In addition to cells invaded by pathogens (either a bacterium, a microorganism, or a virus), killer T cells also target cancer cells.
Adaptive immunity can be active or passive. Active immunity happens when your own body’s B cells generate the antibodies needed to identify the pathogen in the future. This can happen either when you get sick naturally and make antibodies, or when you receive a vaccine containing the pathogen, which then triggers your immune system to make antibodies. Passive immunity happens when you receive the antibodies from another source. This can be either through your mother’s milk when you were nursing, or through the injection of existing antibodies from a different source. [9]
Myths & Mysteries
FALSE
Nope, this won’t work and is a terrible idea! Once your immune system is sensitized to an allergen, you will keep having allergic reactions when you are exposed to that allergen. Allergy shots, or immunotherapy, do desensitize you to allergens, but this must be done under the care of an allergy specialist who will control the quantity, quality and time intervals of these shots. Talk to your healthcare provider for information if you think this may be an approach you are interested in.
FALSE
Some allergic reactions can be deadly. An anaphylactic reaction happens when a very large amount of histamine is released into your system at once causing a massive inflammatory reaction. Symptoms include difficulty breathing, wheezing, stomach pain and cramps, diarrhea, anxiety, swelling of the feet, hands, lips, eyes, and possible loss of consciousness. Death often occurs when airways swell shut. Portable epinephrine injectors, (one common brand is called the EpiPen) are designed to auto inject a hormone called epinephrine, which works rapidly and stimulates the heart, raises blood pressure and reduces swelling in the throat, lips, and face. In Canada, EpiPens are available with or without a prescription. Ask your healthcare provider for advice on whether you should have one available.
NO
If you know you will be coming into contact with a known allergen (visiting your friend who has a dog that you react to, for example), take your allergy medication (often an over-the-counter antihistamine) before you go. This can actually prevent any allergic reaction at all.
FALSE
Absolutely not true, as most allergy sufferers can tell you. Some individuals seem to have more sensitive reactions than others and can have multiple allergies to multiple different allergens. Not all of these allergies will occur at the same time, nor will they all last the same amount of time.
FALSE
Some allergies do, in fact, stick around for your whole life. The good news though, is that many allergies fade away as time passes. It all depends on the allergen and your individual system and sensitivities.
FALSE
Developing allergies in adulthood is relatively common, and in fact nearly half of adults with food allergies had those allergies start in adulthood. While it is very common for adult-onset allergies to happen in your 20s and 30s, perimenopause is a time when many women start to suffer new allergies or have increasingly problematic symptoms to existing allergies. This is caused by the interactions of estrogen and progesterone with the immune system, because estrogen and progesterone bind to the parts of the immune system that trigger allergic reactions.
Citations
[1] https://www.hopkinsmedicine.org/health/conditions-and-diseases/allergies-and-the-immune-system
[2] https://www.mayoclinic.org/diseases-conditions/asthma/in-depth/allergies-and-asthma
[3] https://www.mayoclinic.org/diseases-conditions/anaphylaxis/
[4] https://www.healthline.com/health/histamine-intolerance
[5] Reese I. Nutrition therapy for adverse reactions to histamine in food and beverages. Allergol Select. 2018 Sep 1;2(1):56-61. doi: 10.5414/ALX386. PMID: 31826041; PMCID: PMC6885995.
[6] https://www.healthline.com/health/histamine-intolerance#diet
[7] https://www.mayoclinic.org/diseases-conditions/allergies/diagnosis-treatment
[8] https://www.aaaai.org/Tools-for-the-Public/Conditions-Library/Allergies/Allergy-Shots-(immunotherapy)
[9] https://www.technologynetworks.com/immunology/articles/innate-vs-adaptive-immunity-335116
[10] https://www.aaaai.org/Tools-for-the-Public/Allergy,-Asthma-Immunology-Glossary/Immunoglobulin-E-(IgE)-Defined
[11] Branco, A., Yoshikawa, F., Pietrobon, A. J., & Sato, M. N. (2018). Role of Histamine in Modulating the Immune Response and Inflammation. Mediators of inflammation, 2018, 9524075. https://doi.org/10.1155/2018/95240757
[12] Benly. P (2015) Role of Histamine in Acute Inflammation Journal of Pharmaceutical Sciences and Research Vol. 7(6), 2015, 373-376
[13] Weidenhiller M, Layritz C, Hagel AF, Kuefner M, Zopf Y, Raithel M. Histaminintoleranz-Syndrom (HIS): Vielfalt der Mechanismen von physiologischer, pathophysiologischer und toxischer Wirkung und deren Unterscheidung [Histamine intolerance syndrome (HIS): plethora of physiological, pathophysiological and toxic mechanisms and their differentiation]. Z Gastroenterol. 2012 Dec;50(12):1302-9. German. doi: 10.1055/s-0032-1325487. Epub 2012 Dec 7. PMID: 23225559.
[14] https://www.webmd.com/allergies/what-are-histamines