What is Oral Health?
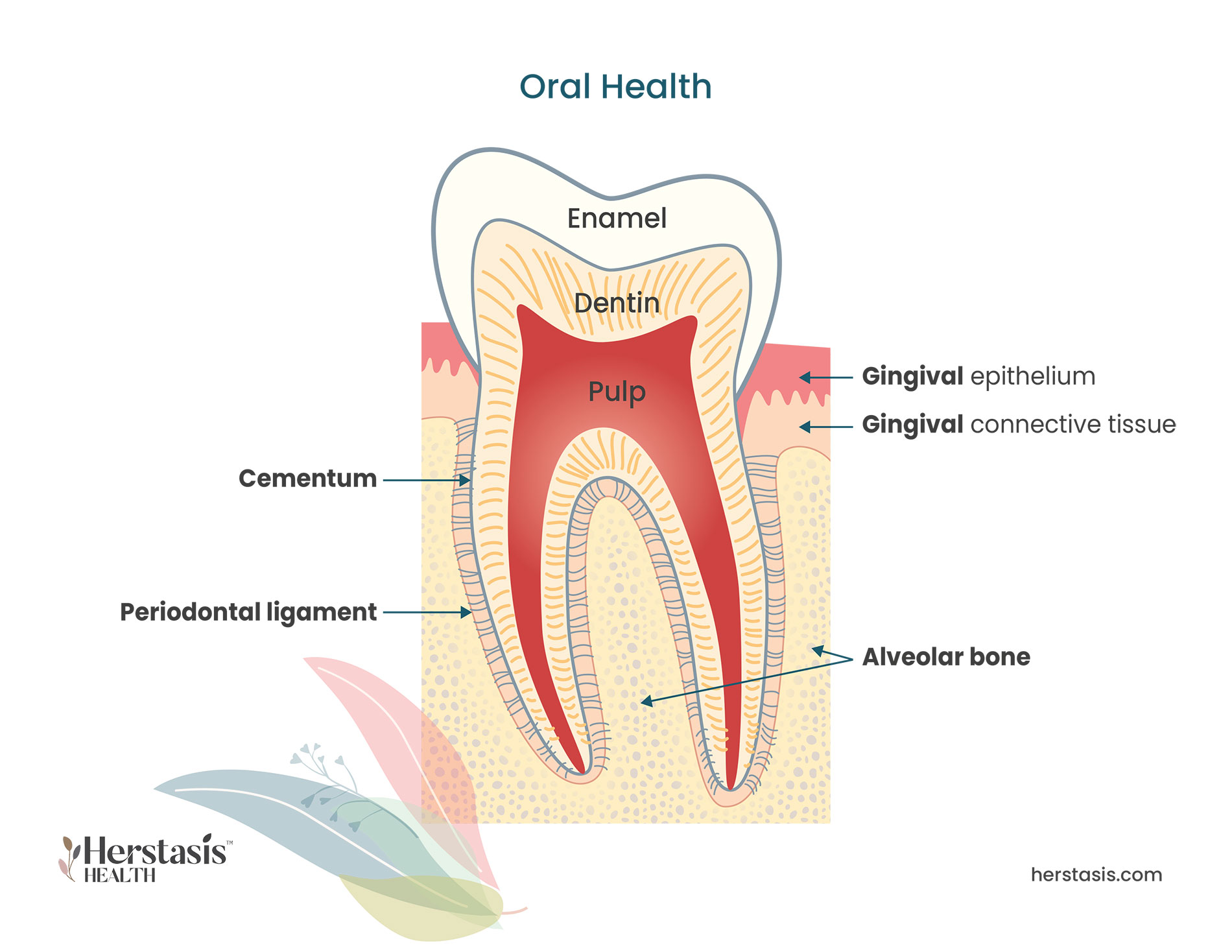
Healthy gums fit snugly around teeth and act to hold them securely in place. They are firm and have a colour ranging from pale pink to dark brown. Periodontitis is the formal name for gum disease, and it starts by damaging the soft tissues of the gum. Without treatment, periodontitis can go on to destroy the bone that supports your teeth, leading to loose or lost teeth. [1]
The oral mucosa, which is the soft tissue lining the mouth (including the insides of your cheeks and lips), and the salivary glands both contain estrogen receptors. This means that hormone fluctuations associated with the menopausal transition can affect the health of your mouth, gums, and teeth. Increasing age combined with decreasing estrogen levels disproportionately increases women’s risk of oral disease, among other conditions. [2] [3] However, some studies have concluded that the menopausal transition does not appear to significantly influence the severity of periodontal disease and tooth loss. [4]
Oral health problems overall are predominantly driven by a decrease in the production of saliva. This leads to an increase in tooth cavities, inflammation of the gums (atrophic gingivitis), gum disease (periodontitis), mouth sores (oral ulcerations) and bone loss in the jaw (osteoporotic jaws). [3] [5]
Other oral health problems include burning mouth syndrome, dry mouth (xerostomia), and bad tastes in the mouth (dysesthesia) are all discussed in the Burning Mouth Syndrome section.

Self-care & Natural Remedies for Oral Health
There is a lot that you can do to keep your mouth, gums, and teeth healthy on your own. Practice the following to maintain a healthy mouth and strong teeth:
- Brush teeth with a soft toothbrush thoroughly twice a day and floss daily between the teeth to remove dental plaque.
- Use mouthwashes containing chlorhexidine digluconate, which is an antiseptic agent with topical antibacterial activity. Your dentist, healthcare provider, or pharmacist can recommend an over-the-counter brand of mouthwash for you. Regular brushing and the use of chlorhexidine digluconate reduce the accumulation of dental plaque, and is known to prevent cavities, particularly root cavities that are common in older individuals.
- Drink fluoridated water.
- Brush your teeth with fluoride toothpaste.
- If you are able, visit your dentist at least once a year, even if you have no natural teeth or have dentures. At these visits ask your dentist to take a full clinical history so you have a baseline of your dental and mouth health. This includes examining your oral mucosa (the soft tissues inside your mouth) and evaluating your salivary flow. Have regular X-rays taken.
- Do not use any tobacco products, and if you currently smoke, quit.
- Limit the amount of alcohol you drink.
- If you have a dry mouth, check your medications – talk to your healthcare provider to see if that could be the cause. If your dry mouth continues, stay hydrated, chew sugarless gum, and take extra care to avoid tobacco products and alcohol.
- See your doctor or a dentist if you have sudden changes in taste and smell. [6]

Therapy & Treatment for Oral Health
At age 40 find a reliable, educated primary care provider familiar with recognizing and treating symptoms of perimenopause and menopause. The North American Menopause Society provides a list of menopause practitioners here.
There are no guidelines specific to oral health care in perimenopausal or postmenopausal women. [3] However, following the basics of oral health care as described in the Self-Care section above will give you the basic guidance for good oral health. Talk to your healthcare provider about your oral health and any concerns you might have. The best case scenario would see both your healthcare provider and your dentist having awareness of your oral health and your menopausal status, especially your reproductive age. [2] [3]

Hormone Therapy (HT) for Oral Health
The use of hormone therapy to help manage oral health is controversial because no clear relationship has been seen between HT and improved oral health. [2] [3] [5] [7] [8] However, there are indications that HT can be helpful. For example, some studies reported significantly greater occurrences of periodontitis in post-menopausal women who were not using HT compared to women who had not entered the menopausal transition. Other studies showed that post-menopausal women using HT and premenopausal women had similar periodontal status. The Women’s Health Study assessed 42,171 post-menopausal women and found that the overall risk of tooth loss was 24% lower in current HT users than in non-users. [5]
Some studies have found that women who start using HT report improvement in their quality of life, including reduced oral discomfort. These studies propose that increased saliva secretion is the main reason for the improvement of oral discomfort. These studies also show that saliva production amounts in pre- and post-menopausal women does differ based on estrogen levels. [5] Other studies, however, show that women’s salivary gland function is not significantly influenced by either menopause or HT. [9]
It appears that the effect of HT on oral health varies among women – some women benefit while others do not seem to be affected and don’t show improvement. Researchers continue to call for better designed, well-controlled, long-term randomized clinical studies. The results from these studies would form the basis of better clinical guidelines for perimenopausal women’s oral health. [3] [5]
The Science
Myths & Mysteries
MYTH
Unfortunately, this is not true. While gum disease can definitely cause bad breath, it is not the only cause by far. If your bad breath or a bad taste in your mouth doesn’t go away, talk to your dentist or your healthcare provider to see what the cause could be.
MYTH
Gum disease is painless so there aren’t any obvious indicators that you are experiencing gum disease. Your dentist can help determine if you are at risk. If your gums are red and sore and / or bleed easily you are at an early stage of gum disease and the condition can be reversed with the help of proper dental care.
MYTH
No, unfortunately gum disease is very common. The US Centers for Disease Control and Prevention states that 50% of adults over the age of 30 have some form of gum disease. You can help keep your gums healthy by practicing good dental hygiene and brushing and flossing regularly to remove the buildup of plaque on your teeth.
Citations
[1] https://www.mayoclinic.org/diseases-conditions/periodontitis/symptoms-causes
[2] Friedlander AH. The physiology, medical management and oral implications of menopause. J Am Dent Assoc. 2002 Jan;133(1):73-81. doi: 10.14219/jada.archive.2002.0025. PMID: 11811747.
[3] Suri V, Suri V. Menopause and oral health. J Midlife Health. 2014 Jul;5(3):115-20. doi: 10.4103/0976-7800.141187. PMID: 25316996; PMCID: PMC4195183.
[4] Alves RC, Félix SA, Rodriguez-Archilla A, Oliveira P, Brito J, Dos Santos JM. Relationship between menopause and periodontal disease: a cross-sectional study in a Portuguese population. Int J Clin Exp Med. 2015 Jul 15;8(7):11412-9. PMID: 26379957; PMCID: PMC4565340.
[5] Dutt P, Chaudhary S, Kumar P. Oral health and menopause: a comprehensive review on current knowledge and associated dental management. Ann Med Health Sci Res. 2013 Jul;3(3):320-3. doi: 10.4103/2141-9248.117926. PMID: 24116306; PMCID: PMC3793432.
[6] https://www.cdc.gov/oralhealth/basics/adult-oral-health/tips.html
[7] Geurs NC, Lewis CE, Jeffcoat MK. Osteoporosis and periodontal disease progression. Periodontol 2000. 2003;32:105-10. doi: 10.1046/j.0906-6713.2003.03208.x. PMID: 12756036.
[8] Grodstein F, Stampfer M. The epidemiology of coronary heart disease and estrogen replacement in postmenopausal women. Prog Cardiovasc Dis. 1995;38:199–210.
[9] Ship JA, Patton LL, Tylenda CA. An assessment of salivary function in healthy premenopausal and postmenopausal females. J Gerontol. 1991 Jan;46(1):M11-5. doi: 10.1093/geronj/46.1.m11. PMID: 1986036.
[10] https://www.nature.com/articles/bdjteam2015123
[11] Suba Z. Gender-related hormonal risk factors for oral cancer. Pathol Oncol Res. 2007;13(3):195-202. doi: 10.1007/BF02893499. Epub 2007 Oct 7. PMID: 17922048.
[12] https://www.mayoclinic.org/diseases-conditions/mouth-cancer/symptoms-causes/syc-20350997